A new open protocol delivers a high-quality tool for human in vitro modeling
Asst. Prof. Muwan Chen developed a new open-access protocol describing a whole new recipe for making a long-term in vitro culture that with high precision mimics the in vivo situation.
Studying the brain down to a single-cell stage is what makes in vitro human modeling very attractive when understanding and treating neurological diseases. A new open-access protocol describes a whole new recipe for making a long-term in vitro culture that with high precision mimics the in vivo situation. With strong reproducible capability and cost-effectiveness, the protocol can become an important tool for moving the research field forward.
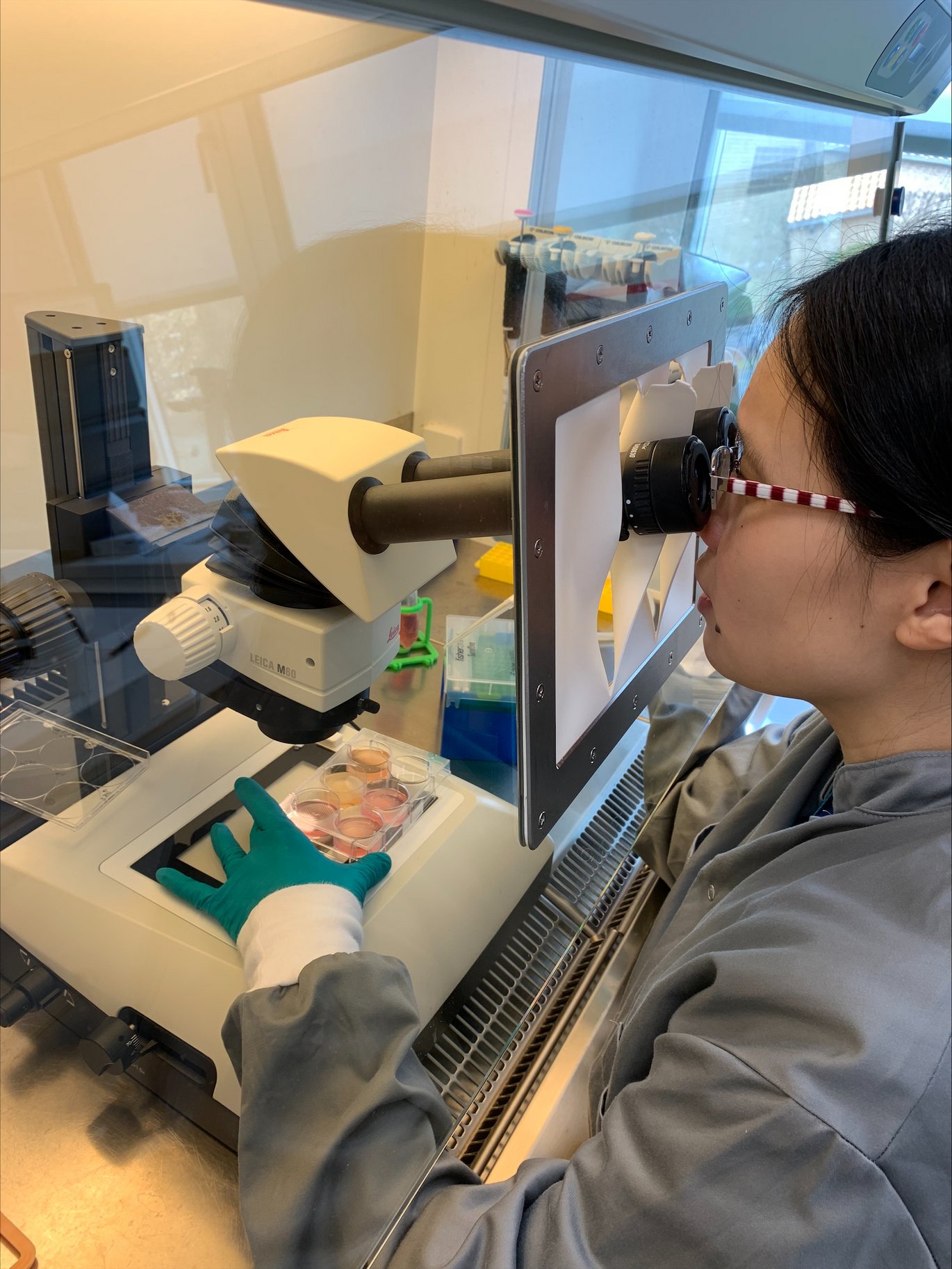
Muwan Chen opens a small incubator. The temperature inside it is 37 degrees Celsius – similar to normal body temperature. She carefully takes out a plastic well and places it under the microscope. With a high level of detail, she studies the format, structure, and quality of the 1200 human organoids steadily growing in the well.
“They are not quite there yet, but they are developing really nicely,” she explains.
Assistant Professor Muwan Chen knows exactly when her organoids have reached their maturity. She has worked with developing cell cultures since her Ph.D. where she focused on developing three-dimensional (3D) culture for bone tissue engineering for clinical application use. Now she has invested all her passion in developing a protocol on how to use human stem cells to create different parts of the human brain in Mark Denham’s Lab at DANDRITE:
“Neurological diseases affect different parts of the brain, so there is great interest in making tissue that recapitulates the different parts that are affected. So, in our lab, we started focusing on the midbrain, because developing dopaminergic neurons for the treatment of Parkinson disease is the main focus in our lab and it is still very challenging in the scientific field,” says Muwan Chen.
The midbrain controls many key functions of the body, from vision, hearing, motor control, sleep, and temperature regulation, owing to the continuous release of dopamine in the neurons.
Midbrain dopaminergic neuron degeneration is one of the main causes of Parkinson’s disease, but many other human disorders are also impacted by abnormal dopamine, including drug addiction, autism, and schizophrenia. So, recapitulating this particular part of the brain has become extremely relevant for identifying new diagnostic methods, studying disease development, and developing drug treatments for a wide range of neurological diseases.
Smaller organoids, higher quality
The growing midbrain organoids placed under Muwan’s microscope are thus part of a fast-growing trend that has developed throughout the last decade, because of their potential for manipulation and in-depth biological studies. However, using organoids as a research object also comes with an extremely high demand for reproducibility and uniformity:
“Because imagine you want to do a repeated drug screening. You take some of the organoids out, and they behave differently. How can you trust which part the result is true? So reproducibility is very important – they must be very similar from one organoid to another, from one batch to another batch,” she states.
Despite years and years of testing and cultivating, the high demand for reproducibility is still what keeps the organoid field from moving forward. Going through the many publications that have been published throughout the years one specific trait of the organoids seems to be repeating itself: a dead center. Muwan Chen explains why:
“Just like the cells in the body, the organoids need to have nutrition coming in and waste going out to be viable. Transport relies on diffusion and if the distance between the center of the organoid and the outside is too large, this will delay or block the process and as a result, the center of the organoid will become necrotic and the cells in the center will die.”
To conclude: If the organoids are too big, the cells in the center are less likely to survive, and hence not suitable for long-term culturing or disease modeling. So, what is the optimal size?
2 years of testing collected in a step-by-step recipe
The answer might be found in the wells carefully stored and maintained in Muwan’s incubator. Through the last two years of testing, Denham Lab with Muwan in front has reached a result, that is both cost-efficient, long-lasting, and most importantly reproducible both within the same batch and across batches.
“We have insisted on making them small from the beginning. We have changed the size of the wells and we have tested constructs ranging from 50 cells to 1000 cells, while other labs work with up to 20.000 cells. Our result is long-term in vitro culture that mimics the in vivo situation and thus neurons that also stay mature and viable for a longer period – without the necrotic center.”
Every single step has been carefully noted and described in detail – from the size of the well, the changing of media, and the equipment needed to study the development. All with the aim of making a “plug and play”-recipe for other labs to use:
“You can think of our protocol like a base recipe where you can add what you're interested in to make your own “flavor”, hence you can customize it to fit with different research focuses,” Muwan explains.
Bridging the gap between animal testing and human-relevant set-ups
Given its reproducibility, high level of in vivo mimicry, and cost-efficient way of maintaining the culture, makes it extremely relevant to use as a validation or even replacement of the use of animals in drug testing.
“Animal testing can be both ineffective and expensive, so in this case, the human organoids would be a great system to be used for drug testing since we can test the drugs in a 3D environment which can better mimic in vivo and on a human material,” Muwan explains.
One of the protocol’s first users is the spin-out company, Teitur Trophics from Aarhus University. The company has developed novel peptide therapeutics that have been tested and shown great efficacy in several animal models of neurodegeneration, including Parkinson’s disease. CSO of Teitur Trophics, Anders Dalby explains how using organoids has provided further confidence in the efficacy of the Teitur peptides:
“The use of animal models comes with some challenges including their translatability to patients. Fortunately, Teitur was given the opportunity to validate their mechanism in Muwan’s Parkinson’s patient dopaminergic organoids, as a way of bridging the gap between in vivo proof-of-concept studies and human-relevant setups.”
He has no doubt that human organoids will be an essential part of future research on neurological diseases:
“Human organoids serve as a highly valuable in vitro tool for preclinical drug testing in disease areas in which animal models have poor translatability to patients including neurological disorders,” he states.
It is Muwan’s hope that many more labs will find the recipe useful and see the great perspectives in using organoids for disease modeling and testing.
“I am particularly happy with the sharing part of our knowledge,” Muwan concludes and adds:
“With our protocol, we have set the stage and put together a system, that both saves time and is easy to use if you want to include 3D organoids in your research,” Muwan explains.
The protocol is part of the Open Discovery Innovation Network (ODIN), funded by the Novo Nordisk Foundation, that connects academia and industry through open innovation projects for better and faster drug discovery.
- The protocol was published in STAR Protocols in July 2023
- Link to protocol
- Read more about ODIN
